Chicago’s public health goals are shifting toward battling crime, tenement housing and other stubborn social concerns. Nearly a year of data-driven community discussions have led the city’s health professionals to look beyond their traditional roles treating infections, substance abuse and other conditions.
“There are chunks of population in Chicago that are just suffering tremendously, and we just aren’t targeting our resources in the right way,” says Jaime Dircksen, deputy commissioner of the Chicago Department of Public Health. “We started this process with equity in mind, and with the goal of achieving equity across the city. I think having that lens really led to people feeling comfortable talking about some of the causes of these problems.”
Attacking these problems meant coming up with an approach other city departments would support in their own programs. Now the Healthy Chicago 2.0 plan is being circulated in City Hall for unveiling in late fall. Its priorities emerged in a community-driven process, developed for public health agencies with the federal Centers for Disease Control and Prevention.
“This plan is not the health department’s plan, it’s the city’s plan. Everyone plays a role in improving the health of the city,” Dircksen says. “We will be meeting with city department heads to make sure they understand what’s being put forth in the plan and will champion the plan. Then we’ll convene the interagency council of city agencies and share with them the draft of everything,. We’re identifying the opportunities where we can create synergy. “
Data to the people
Some 800 people contributed to the goal-setting process, a quarter of them in 10 working groups that set objectives and strategies. A data-intensive approach kept this potentially unwieldy goal-setting effort on track.
Percent of live births in which mother began prenatal care during 1st trimester, 1999 – 2009 (Chicago Health Atlas)
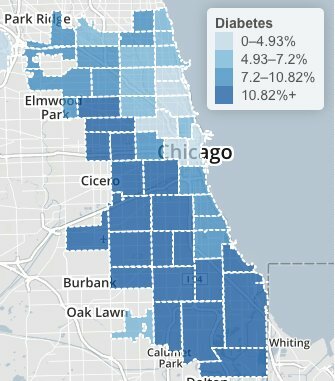
Public-health staffers gave work-group volunteers a thick stack of statistics on births and deaths, hospitalizations and personal habits. They mapped health outcomes by neighborhood, conducted survey research and adopted novel ways to probe the underlying causes of chronic diseases.
Finally, they faced down the realities of an austere 2016 city budget. The health department controls only $149 million directly, a 4 percent cut. Most of that is set aside for AIDS, women’s and children’s health, mental-health and emergency services.
“There’s a strong paradox constantly at work,” says Nikhil Prachand, the health department’s director of epidemiology and public health informatics. “It’s impossible to narrow down the priorities, but if you don’t have a lot of money it should be easy to narrow down the priorities. “
Smart Chicago will play a role in measuring the plan’s success. The city will use the Chicago Health Atlas website to mark progress toward goals for 2020.
“We will have a dashboard of indicators monitoring every action area,” Dircksen says. A website update will “really dive deep into community area data so that the community can see progress,” she says. “Community-based organizations can use it as a resource for funding opportunities and monitoring their own work.”
Planning began last year with surveys in English and Spanish, asking broadly about a healthy environment. Residents across the economic spectrum united around safety and access to healthy food as citywide needs. Yet there wasn’t much agreement on neighborhood needs.
In areas under economic stress, crime emerged as the top priority. In affluent areas – nearly half the sample – respondents were more concerned about the built environment as a local issue. The widest gulf was in access to education, based on agreement with statements like, ”Schools in my neighborhood have what they need to provide a high quality education.”
Tackling broader issues like safety, Dircksen argues, takes “understanding that people aren’t going to parks because they don’t feel safe, they’re not well lit, there’s trash all over the place, that’s where the gang violence happens — then thinking out how to respond to those issues.”
Percent of occupied crowded housing units, 2007-2011 (Chicago Health Atlas)
Root causes
Five panels probed more deeply into the equity questions. “They did a focus group with our hotline volunteers to hear the stories they’ve heard,” says John Bartlett, executive director of the Metropolitan Tenants Organization. “And they asked about their lives also, because many of them are tenants.“
University of Illinois at Chicago students scored the responses, along with content from a half-dozen StoryCorps oral histories. They found common themes – problems navigating mainstream society and a sense of powerlessness. Again, health issues were linked to larger social problems.
“For example, mold will trigger asthma,” Bartlett says. “We are continually counseling parents whose children have uncontrolled asthma, informing them of steps they have to take to get their landlords to make the environment safer for their kids. Oftentimes landlords can be recalcitrant about that.
“We will inspect units for things like paint dust, and if there is, work with the health department to get a city inspection and encourage families to get their kids tested,” he adds. “And bedbugs are definitely a stressor in people’s lives. They blame themselves, but it’s not anyone’s fault. These creatures are just hitchhiking all over the place.”
The next step was to share the results with local health advocates. Many were frustrated at the lack of money, equity, attention and political will to take on core issues. And they saw traps ahead for clients navigating Affordable Care Act enrollment and mental health clinic closures.
“We were happy because the city was making efforts to be accessible and to be inclusive of the disabilities community,” says Gary Arnold, spokesman for Access Living, which hosted one of the advocate forums.
Local Pubic Health System Assessment (Chicago Department of Public Health)
Opportunities and threats
In one exercise, service providers scored the local health system using a CDC-approved framework. Working groups saw electronic health records posing opportunities for data sharing and monitoring, and threats from uneven adoption and stale information.
Health advocates saw new communication tools as potential threats, raising access barriers or triggering changes in brain development and socialization. But technology also was part of the solution: Ideas included wrist monitors, health provider networks and a 2-1-1 phone line to take health and human service calls.
“We ended up with 50 priorities, and they’re all very important,” Dirksen says. Grouping them yielded a more workable list of 16 themes, which were ranked by public and private stakeholders in the Partnership for Healthy Chicago. The city convened 10 expert panels this summer to draft objectives and strategies in key areas.
HEALTHY CHICAGO 2.0 ACTION AREAS
- Access to healthcare and human services
- Behavioral Health
- Chronic disease prevention and control
- Community development
- Data & Research
- Education equity
- Infectious Disease
- Maternal, Infant, Child and Adolescent Health
- Partnerships and Community Engagement
- Violence and Injury Prevention
“The first thing is laying out the roadmap then creating the will to fund it,” says Bartlett, who joined the community development team. “If we’re serious about having a healthier Chicago we need to look at prevention. All the departments dealing with housing should be on the same page looking at health as part of the decision-making process. How do we make sure Chicago housing is affordable and healthy? It’s not good to have only one without the other. “
Distributed network
The teams will reconvene next month to draft detailed plans. Eight final themes will mirror the action areas, with data and engagement as strategies throughout. “We can’t do any of this work without having the data to inform it, the research to gather additional data – and it’s an all-hands-on-deck effort,” Dircksen says.
Data will help make the case for funds, and track whether they’ve been spent wisely. “Community development is focused primarily on capital improvements – improving CTA stations, rehabbing schools, building structures,” Prachand says. “We have been able to assess the health of the city’s commercial areas and offered a number of metrics. We can monitor over time and give feedback whether these capital improvement projects and grand plans are having some impact on people. “
The plan calls for more community input, in projects such as locating new Divvy bike stations on the South Side. “How do you know where the next best place is? Not necessarily by looking at a map,” Dircksen says. “They have to talk to the community leaders and stakeholders. We’re talking about the public health planning and transportation planning worlds coming together, and working together to identify mutual benefit and priorities.”
The city will count on private agencies to take on some of the burden. “Funders are wholly committed to obesity, metal health, access to care, violence prevention,” Dircksen says. “They appreciate and understand housing is health care. But then they’re giving across the city, not making a great impact, and not necessarily using evidence-based strategies. How do we work with them to make sure they understand what the evidence is and what does work, and concentrate their efforts in places or with populations which we know need the most?”
“It’s our job to mobilize and motivate the community to be a part of this,” she adds. “By 2020 we expect to achieve all the things we’ve laid out. I think with this process we will have a lot of engagement come launch because people will have been involved throughout the process. There’s a lot of evidence that when you engage people from the very beginning, they’re more likely to buy in, they’re more likely to act.
“If we don’t address environment and community conditions and access to care, we’ll never be able to impact the lives of people,” she adds. “At the forefront we will focus on those root causes of why folks are overweight, why they’re smoking, why they aren’t caring for their chronic conditions or their mental illness, or why pregnant moms can’t get prenatal care or can’t deliver a healthy baby.”
This plan, Healthy Chicago 2.0, is utilizing the Mobilizing for Action through Planning and Partnerships model, which was developed by the Centers of Disease Control and Prevention (CDC) and the National Association for County and City Health Officials. Healthy Chicago 2.0 is a four year plan that will outline goals and strategies for Chicago Department of Public Health (CDPH) and public health stakeholders to implement and work towards improving the health of Chicago residents and communities.